

Be in the Know
Elevate your industry knowledge with yoga articles and insights crafted by experienced industry experts
Mindfulness could be described as one of the most popular movements and trends of recent times. This ubiquitous term has found its way into almost every echelon of modern living. Everyday people, professional athletes, businesses and even the NHS have embraced mindfulness as a means of tackling stress, depression, anxiety and improving overall wellbeing.
Mindfulness has almost become an industry unto itself and it’s embedding into mainstream consciousness has been rapid, to say the least. There’s no shortage of educational institutions offering courses and qualifications in it, wellbeing practitioners (life coaches et al) offering mindfulness training as part of their services and thousands of apps offering guided mindfulness meditations available.
To the latter point, recent Google data suggests that searches for “mindfulness apps” grew 65% year-on-year, while more than 2,500 meditation apps have launched since 2015 alone. Further to that, spending on meditation apps has continued to grow year-on-year, reaching £148 million in 2019. Putting it simply, it’s big business.

Alongside the wide range of potential benefits listed above, mindfulness has also been heavily linked to pain relief, particularly when it is long-lasting, or chronic to use common parlance. In this article we’ll take a close look at what mindfulness actually is and whether or not mindfulness-based pain management programmes (MBPMs), mindfulness-based stress reduction (MBSR) and other associated techniques can have a tangible benefit.
Before we explore the science of mindfulness and the studies around its relationship to chronic pain relief, it’s important to define what mindfulness actually is and also what it isn’t.
A very simple definition is that: mindfulness is our ability to pay more attention to our thoughts, feelings and the wider world. It’s a ‘process’ of paying more attention to the present moment. While that may sound very simplistic and straightforward, mindfulness (and being mindful), isn’t just a case of stating the obvious, saying to yourself, ‘the sky is blue’ or ‘I’m feeling tired’. It’s about being fully engaged with whatever is happening in the present moment and that goes for both positive and negative emotions and sensations. It’s less so about ignoring negativity or an uncomfortable physical sensation, and more about recognising it and not letting it overwhelm us.
One of the biggest misconceptions about mindfulness or a mindfulness practice is that it’s some incredibly intricate or all-consuming spiritual thing we have to involve ourselves in. Yes, mindfulness is a central part of some religions, particularly Buddhism, and it’s often intrinsically tied to practices such as yoga and tai-chi. However, it can be a standalone thing used by anyone, regardless of temperament, religion, or belief system.

Another misconception or misnomer is that mindfulness is a state of mind that we enter in to. Instead, the literature, both religious and scientific, suggests that this isn’t the case. Mindfulness or being mindful is better viewed as a habit, as a way of living. If it helps to better ground things, think of it in the same way you would a diet or exercise programme, it’s just something you ‘do’ and engage with.
Just as they are numerous purported benefits of engaging in a regular mindfulness practice, there are almost as many, if not more, ways to be mindful. Without a doubt, the most popular and most marketed is mindfulness meditation. All it takes is a glance at the App Store or a Google search to reveal an almost overwhelming amount of results. The likes of Calm, Headspace, Buddhify and Tricycle Magazine often appear at the top of many published lists but they are just several popular choices out of thousands.
Mindfulness meditation is the most universally popular and mainstream form of engaging in a mindfulness practice, but just as the definition of mindfulness is quite broad, mindfulness meditation can often be viewed this way. Essentially, mindfulness mediation involves the following steps:
Being in a quiet place – the stereotypical image of a meditator is someone sat in padmasana (lotus pose) on a cushion or mat, however, mindfulness meditation can be performed seated on a chair, walking, standing or even lying down.
Control the breath – A typically-used technique is to breathe softly in and out through the nose and mentally note when an inhale occurs and then when an exhale occurs. For those who are struggling for concentration, methodically counting in- and exhales can help.
Observe emotion and sensation – the crux of mindfulness meditation is to acknowledge what is happening to the body and in the mind without reacting to it or judging what is happening.

An important part of mindfulness meditation is always ‘returning to the breath’ and it’s a phrase used commonly by meditation teachers and instructors. It simply means that when distractions occur or sensations and thoughts arise (and they will, even for the most ardent), instead of clinging to what’s happening, you should just re-focus your attention on breathing and start the process again. As grandiose as it may sound, with mindfulness meditation, there is no right or wrong, there is just what occurs.
One of the many reasons why mindfulness-based techniques have been explored as a possible treatment for pain relief is because of just how many people are affected by chronic pain. This naturally puts a tremendous amount of strain on the NHS, but there’s also the financial implication to businesses and the wider economy to consider.
Perhaps most importantly, for those dealing with chronic pain (moderate-severe intensity lasting greater than six months), the psychological and emotional impact is often hard to quantify. Mentally, dealing with pain on a long-term basis can be incredibly debilitating and demoralising.
In terms of numbers, there are varying and often conflicting reports about just how many people in the UK live with chronic pain. Some estimates, based a collection of studies, suggest that one-third to one-half of the UK’s population is affected by chronic pain and this equates to around 20-30 million people.
Other studies, however, would place this figure closer to 8 million, so in terms of achieving a consensus on the true number, you can see there’s a lot of variance between studies.
Regardless of the actual figures, it’s clear that people in their millions are being affected on a daily basis, so it’s easy to understand why mindfulness-techniques are being considered, particularly if medication has been over-prescribed and proven ineffectual or surgical interventions aren’t possible.
While teaching mindfulness techniques to a client or patient isn’t devoid of monetary cost, it has the potential to be an incredibly effective cost-saving measure in the long term. What it also does is make the client or patient more self-sufficient, they’re being given tools and resources that they can revisit time and time again, as needed. That alone can be a very empowering thing.
For context, while the exact cost to the NHS of treating chronic pain is unknown, it’s estimated that it’s currently £4 billion a year. It’s a figure that has dramatically surged upwards in recent decades. For comparison, the cost per year back in 1993 only amounted to £500,000.
As previously mentioned, mindfulness techniques and mindfulness meditation have often closely been linked to religious and spiritual practice, particularly Buddhism. While exploration into the scientific benefit of using mindfulness for pain relief is in its relative infancy, for thousands of years, Buddhist monks have extolled the virtue of mindfulness as a means of altering the experience of pain.
Most notably, and often cited, is The Arrow (or Sullatta Sutta). It’s this ancient teaching that encourages meditators to fully experience a sensation and then effective ‘let go’ of the attachment to this. Advances in neuroimaging have meant mindfulness’ effect on the brain and its response to pain mean are no longer talked about in a purely subjective context. It’s now possible to firmly assess whether or not mindfulness techniques are effective tools for pain relief.
Mindfulness-based techniques such as MBSR and MBPM have been the focal point of several recent studies and the results are interesting, to say the least. For a bit of background, mindfulness-based stress reduction was a programme originally developed by Jon Kabat-Zinn in the ’70s. Kabat-Zinn is a best-selling author, scientist and mediation teacher, perhaps one of the most famous and revered in the West.
He founded the now world-renowned Mindfulness-Based Stress Reduction Clinic in America has his original 8-week MBSR course continues to be used and adapted to this day. The programme itself explores various mindfulness meditation exercises and techniques with a view to helping participants really drill down into what’s happening in their bodies and minds.
Researchers from the University of Washington and the Group Health Cooperative recently conducted a study on 342 participants aged between 20 and 70 who were suffering from chronic low back pain. Groups were formed, the first would continue their existing programme of treatment, the second would use mindfulness-based stress reduction and the third would use cognitive behavioural therapy techniques (CBT).
At 26 weeks it was found that participants using both MBSR and CBT saw a greater improvement in function and a lessening of back pain symptoms than those who persisted with their standard programme of care. Interestingly, those using CBT techniques did not see any further improvement past 26 weeks, while those who continued with MBSR saw improvement up to 52 weeks.
Speaking about the results, Josephine Briggs, director of the National Centre for Complementary and Integrative Health (NCCIH), who commissioned the original study, said: “The results from this research affirm that non-drug/non-opioid therapies, such as meditation, can help manage chronic low-back pain. Physicians and their patients can use this information to inform treatment decisions.”
Another notable study found that less than a week’s worth of mindfulness meditation training was sufficient enough to help participants experience significant reductions in pain intensity. Interesting, however, over a longer period of time the study concluded that reductions in pain intensity did not continue to decrease, rather participants reaction to and engagement with the pain was reduced.
You could conclude, as several other studies have, that a commitment to a long-term mindfulness meditation programme doesn’t actually ever make the pain go away completely, instead it helps participants better manage it on a day-to-day basis. This is very similar to the analgesic effect of certain medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), which are often prescribed to those experiencing chronic pain.
How exactly this occurs has been a point of interest, particularly for Fadel Zeidan, Assistant Professor of Neurobiology and Anatomy at the Wake Forest Baptist Medical Centre in Winston-Salem, America. Zeidan himself has been involved in numerous studies about the field of mindfulness and his work is also often-cited by other researchers and institutions looking at similar subjects.
The focus of this particular study was on the default mode network (DMN), a set of regions in the brain that are active when a person is in a resting state, i.e not focusing on external stimuli. What makes the DMN ‘light up’ is when we are focusing on internal mental states, trying to retrieve memories or imagining things that could happen in the future. The default mode network can be deactivated/suppressed by performing a cognitive task, such as reading for example. Interestingly, previous studies into the default mode network have also shown drug consumption also has this suppression effect.
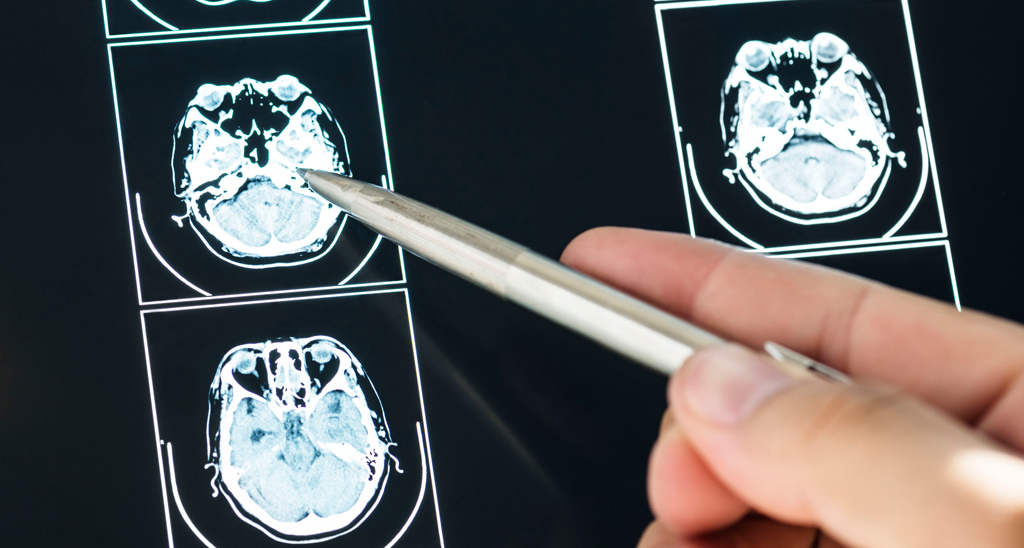
Zeidan found that, of his 76 participants, those who were able to effectively engage with mindfulness mediation were able to cause a greater deactivation of the default mode network. Thus, these participants found themselves less caught up the experience of their own pain. Less and less they found themselves clinging to what was clearly a negative sensation.
Speaking out these findings, he said: “We know we can increase mindfulness through relatively short periods of mindfulness meditation training, so this may prove to be an effective way to provide pain relief for the millions of people suffering from chronic pain.”
What’s evident from the research, and certainly from the marketing of those apps and services who champion mindfulness, is that MBSR and other techniques can provide relief for those suffering from short, medium and indeed long-term chronic pain. It’s important however to understand that mindfulness is not the panacea for a person’s pain. In fact, not everyone is predisposed or completely receptive to mindfulness meditation, so for some, it might simply not be an effective course of action.
For personal trainers, yoga teachers and other exercise professionals, it’s important to never discount the positive impact that diet and exercise can also have on a client. Certain studies around chronic pain tend to only focus on one, or a handful of treatment methods. Wherever possible you should look to use all the tools and resources at your disposal when working with someone suffering from chronic pain.
One possible route could be to upskill and develop your knowledge of mindfulness techniques in order to pass them on to clients. However, as with other situations, if you ever feel like a client’s needs lie beyond your scope of practice, you must always refer them to an appropriate professional, which in most cases will be a GP.
If you would like to learn more about becoming a yoga teacher, or you would like to receive information about our new online yoga teacher courses, please contact our Careers Team on the number at the top of the page.
Back to articlesAnd embrace the rich and vibrant world of yoga
Great news, you're on the list...