Introduction
In the first article, we tackled the basics, looking at the various stages of inflammation and other relevant factors that therapists and other fitness professionals should be aware of. In part 2, I’ll be adding a little more specific information to the inflammatory process, in particular, the time frames involved in the different ways that inflammation can resolve.
Inflammation Recap
As we’ve previously explored, the classic signs of inflammation are heat, redness, swelling, pain, and loss of function. These are manifestations of the physiological changes that occur during the inflammatory process.
The three major components of this process are changes in the diameter of blood vessels and the rate of blood flow through them (hemodynamic changes); increased capillary permeability; and leukocytic exudation.
With an injury of a short duration, an acute, brief inflammatory reaction occurs. With prolonged tissue injury or a persistent infection, chronic inflammation occurs.
The important difference is that chronic inflammation results in the production of vascular granulation tissue which matures into fibrous tissue.
The changes are proliferative in contrast to the exudative changes of acute inflammation.
Acute inflammation may terminate with fibrosis and some proliferation does occur. When the acute stage fails to resolve, the exudative and proliferative phases are often associated together.
The more chronic the inflammation, the more pronounced the proliferative change and the greater the degree of fibrous scarring.
Termination of Inflammation
There are four possible outcomes with regards to the termination of inflammation and this will depend on the cause of the severity of the injury/trauma.
Resolution – Complete restoration of function with scarring only occurring when the original tissue trauma is minimal.

Fibrosis – The degree of residual scarring will vary. Fibrosis may occur from the organisation of fibrin-rich exudate, the mass of cells and fluid that has seeped out from organs or blood vessels. As a therapist or practitioner, you will be involved frequently in dealing with this accumulation of fibrous tissue. Almost all major injuries result in scar tissue formation e.g. ligament and muscle tears.
Suppuration – This is usually due to invasion by pus-forming bacteria (pyogenic) and is a mixture of liquefied tissue, bacteria, inflammatory exudate and other particles.
Necrosis – This stage is without a doubt the most severe and this is when tissue death occurs, e.g. gangrene.
Tissue Repair
There are two ways in which a wound can heal and there are primary or secondary healing, also known as first or second intention.
Primary – This occurs after an injury with minimal tissue loss, for example, if a surgical incision has been made.
0-24 hrs – Neutrophils, the most prevalent type of white blood cells, arrive.
Day 3 – Neutrophil/monocyte infiltration occurs and granulation tissue invades incisional space. Collagen will be present at the margins of the incision. Epithelial cells will then proliferate and thicken.
Day 5 – The space is then filled by granulation tissue and collagen bridges across the affected area. Angiogenesis (new blood vessel growth) occurs. The epidermis recovers its normal thickness and cell differentiation.
Day 14 – Collagen and fibroblast activity continues.
1 month – No inflammatory products are left. The tensile strength of the scar increases over several months.
Secondary healing – When tissue loss is extensive e.g. pressure sore, infarction etc. The repair process is more complicated. Large defects must be filled and there is extensive granulation tissue formed, and more debris removed. Scar contraction may occur.
Wound Healing Types
Essentially wounds can heal in two different ways- a surgical incision with very sharp edges and no bacterial growth heels by something known as first intention. Here the tissues are in very close contact and the resultant scar is very fine and almost invisible.
In some cases, this form of healing is not possible, so for example in a pressure sore or previously infected wound, the edges cannot be brought into contact. Second intention is the way the tissues would repair here and this involves the wound healing from the bottom up by granulation tissue. Whilst this is effective it does result in more scarring.
Healing Factors and Timescales
There are various things that could affect the healing and repair process. It’s important to understand that healing is subject to individual variations.

Here are a few factors to consider:
Age – Young tissues tend to heal more quickly than old ones.
Drugs – Certain drugs e.g. steroids, delay wound healing. Some drugs used in chemotherapy (cytotoxic drugs) slow the growth rate of tumours, but will also affect healing rates.
Disease – People with a systemic disease, for example, rheumatoid arthritis or diabetes, tend to heal more slowly.
Nutrition – Persons who are malnourished do not heal as quickly as those with a healthy diet.
Blood supply – Since blood is the way in which nutrients arrive at the tissues, any condition where blood supply is compromised will result in delayed healing. Examples you will come across include diabetes and peripheral vascular disease.
This is also why tendons and ligaments heal more slowly than muscle tissue (which has a vastly superior blood supply). Fractures of the lower tibia are notoriously susceptible to delay or non-union, owing to the bone having a poor blood supply inferiorly.
Tissue type – The type of tissue damaged dictates the ability to heal. For example, cells of the central nervous system do not regenerate.
Inflammation timeline
Whilst inflammation is often described in three phases it is important to realise that these phases overlap. The diagram below is a useful summary of this.
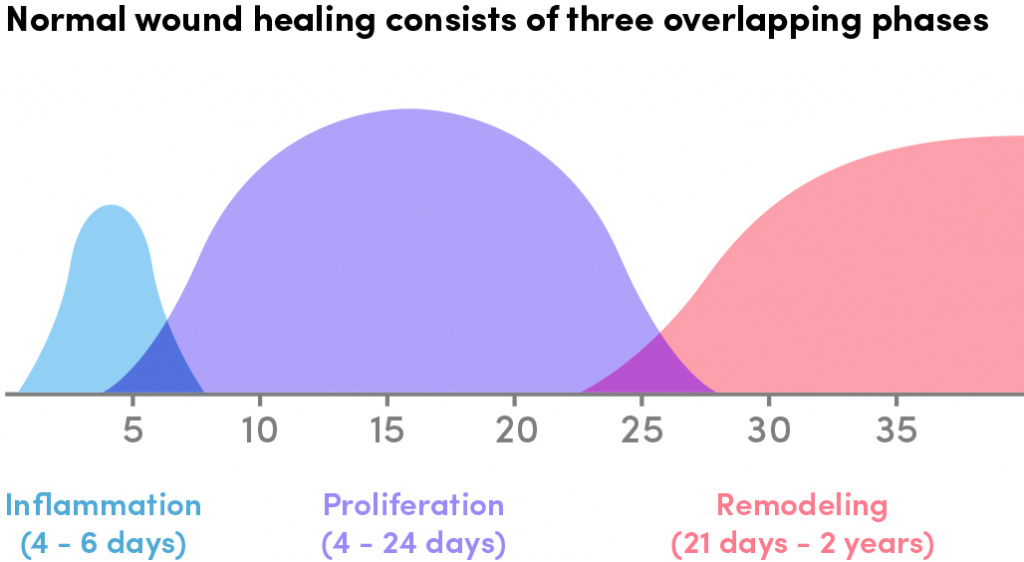
So, for example, if we take a wound at five days, we can see that the acute inflammation stage is dying down and the proliferative phase is on the increase, whereas if we fast forward to 15 days the acute phase has gone completely and everything is in the proliferative phase.


