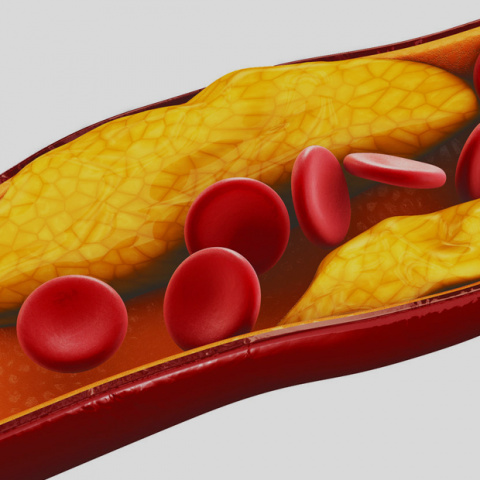
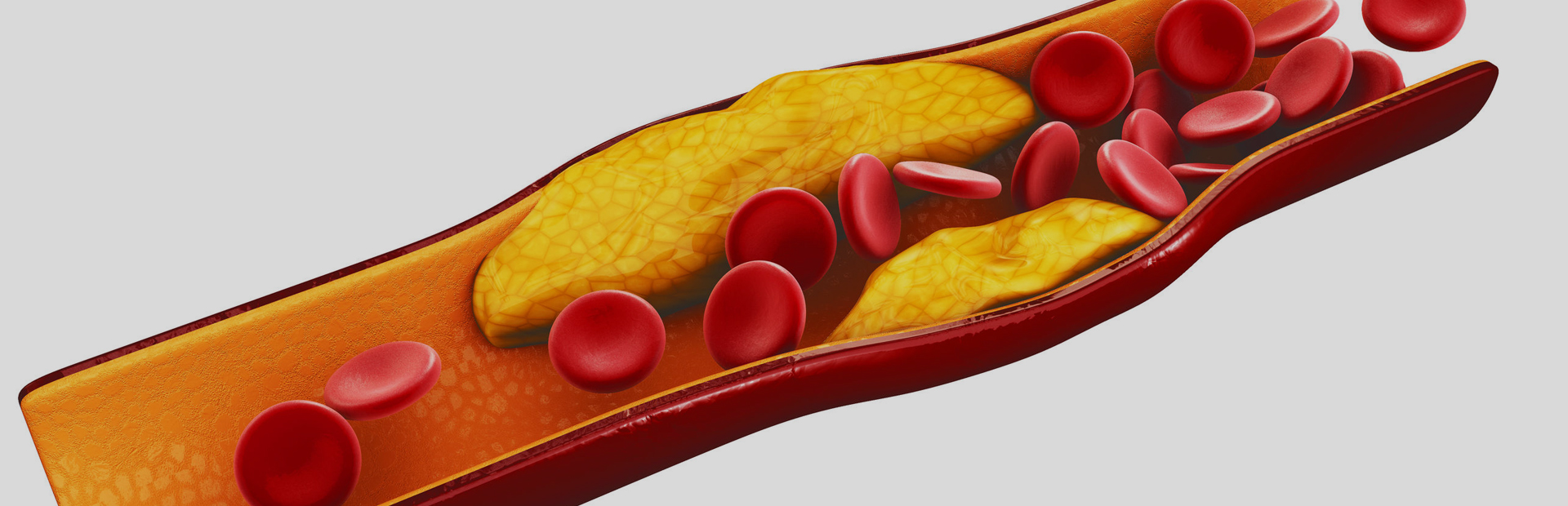
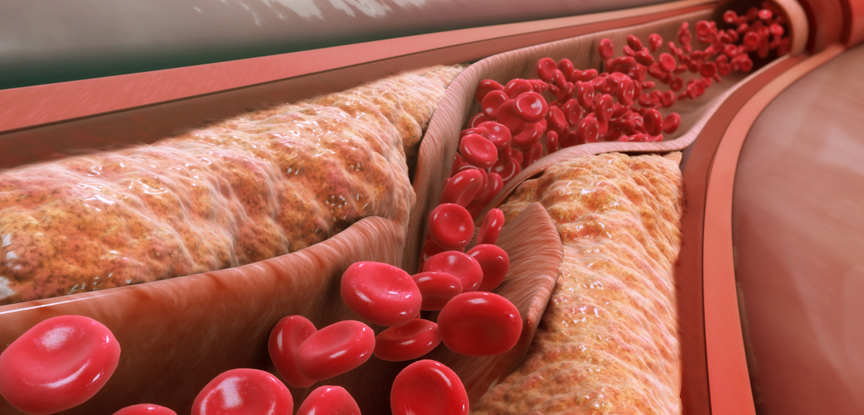
Atherosclerosis is a commonly occurring and potentially serious process where a build-up of fatty deposits and ‘atherosclerotic plaques’ occur within the lumen (the inner space) of the artery. This plaque continues to build-up over time; it impedes the flow of blood through the vascular system and results in an increase in resting blood pressure. When the plaque breaks away from the internal wall of the artery, it can block or ‘occlude’ an already narrow vessel and subsequently restrict blood flow to another part of the body.
When this occurs in the coronary arteries, the person is likely to experience a ‘myocardial infarction’, more commonly referred to as a ‘heart attack’. When the blockage occurs in the brain, the individual is likely to experience a stroke.
It is the severity and location of the occlusion which ultimately determines the symptoms and any associated conditions.
Peripheral artery disease (PAD) is a wider condition which includes atherosclerosis and is associated with occlusions and lesions within the arteries of the lower limbs. Because of the similarities between atherosclerosis and PAD, these two conditions are often described as one and the same.
If atherosclerosis is ignored or left unmanaged, it can lead to cardiovascular disease. Every year it’s estimated that 17.3 million people worldwide die from CVD which equates to 30% of all deaths. Thinking specifically about the UK, it’s not hard to see the sheer weight and strain this has on the NHS. As exercise professionals, particularly those currently working within exercise referral schemes or thinking about upskilling to enter this field, the following makes for essential reading.
Signs and Symptoms
Common symptoms of atherosclerosis include:
Angina Pectoris – occurs when there is an inadequate flow of blood to the heart’s myocardial tissue. Patients suffering from angina report feelings of a tight crushing sensation around the chest that can often radiate along the shoulders, jaw and arms. They may also describe symptoms of breathlessness, nausea and/or sweating. Symptoms can last anywhere from 10 seconds to 30 minutes.
Myocardial Ischaemia – occurs when the occlusion in the artery is significant enough to impede blood flow to levels below those which the myocardial tissues require. Ischemia can occur during periods of challenging activity or stress, but in advanced stages, episodes of very mild exertion may evoke symptoms.
Intermittent Claudication – usually presents itself as pain in the calf, thigh or buttocks during exercise and physical activity. The intermittent nature of the pain is caused by a temporary disruption to the blood supply brought on during physical activity. Other symptoms associated with intermittent claudication include fatigue, limping and lameness while performing seemingly modest physical activities.
As is always encouraged as part of professional development, exercise professionals should strive to develop a wider knowledge of the conditions above.

Medical and exercise professionals should be extremely diligent in identifying those who are at risk of atherosclerosis and its associated conditions, because most patients are ‘asymptomatic’ and exhibit no obvious symptoms. Patients who are considered to be ‘at risk’ of these conditions should be referred immediately to a clinician for further examination.
Basic Pathology
The build-up of atherosclerotic plaque leads to a narrowing of the artery’s lumen and a subsequent rise in intra-arterial pressure. A narrower artery impedes blood flow, which results in less oxygenated blood reaching the heart, muscles and organs.
Additionally, the increased intra-arterial pressure places a greater strain on the myocardial tissue of the heart, because with each heartbeat, the heart requires more force to push the blood through the narrowing vascular system. When the disruption in blood supply is prolonged, the tissue(s) that are deprived of oxygen may experience permanent or temporary damage, depending on the duration and severity of the disruption.
Atherosclerosis of the artery walls is accelerated when higher levels of the ‘low density’ plasma lipoproteins, or LDLs, are consumed in the diet. LDLs become trapped in the wall of the vessel and are subsequently oxidised by the endothelium (lining of the artery). This process ultimately degrades the tone and strength of the artery and increases the risk of further disease to the arteries.
The atherosclerosis process can rapidly progress to other, previously non-diseased arteries throughout the body. In cases where atherosclerosis is unilateral (present on only 1 side of the body), it can also spread to the opposing side of the body in a relatively short space of time. It is, therefore, imperative that individuals who are at risk of this condition are identified and assessed as early as possible, so that the appropriate treatments and interventions can be implemented to prevent the disease from worsening.
Modifiable Risk Factors
Broadly speaking, a risk factor increases the chance of someone getting a particular disease. Therefore, the higher number of risk factors there are, the greater the chance of that disease occurring.

The following risk factors are modifiable which means the client/patient is able to do something about them and lower the risk of atherosclerosis developing into cardiovascular disease. As a fitness professional, it’s your job to make a client/patient aware of these factors and guide them as they tackle the ones applicable to them.
Smoking – approximately 19% of all CVD deaths in people under 75 are smokers.
Hypertension – high blood pressure dramatically increases the workload and physical strain on the cardiovascular system, especially the heart.
Hypercholesterolemia – high levels of cholesterol, particularly LDL cholesterols, accelerate the rate in which atherosclerosis occurs.
Sedentary lifestyle – inactivity reduces the performance and health of the cardiovascular system, especially when combined with other unhealthy practices.
Obesity – an increased presence of adiposity, particularly around the mid-section, dramatically increases the strain on the cardiovascular system.
Diabetes – research has consistently demonstrated diabetes to dramatically worsen the condition of atherosclerosis, even though the precise cause is still unknown. Diabetes can also be considered a non-modifiable risk factor when it is congenital, as in type 1.
Excessive alcohol consumption – moderate alcohol intakes can help to manage atherosclerosis because alcohol reduces the viscosity of the blood and increases HDL concentrations. When alcohol consumption is excessive however, HDL levels are reduced and greater low-density plasma lipoproteins (LDL) circulate with cholesterol – this has an adverse effect on the health of the cardiovascular system.
Stress – research undertaken in this area has revealed that the rate at which atherosclerosis occurs in those exposed to high levels of chronic stress is greater than that in individuals who consume a diet rich in fat. Hormone responses, especially cortisol are believed to be significant in the acceleration of this process.
Non-Modifiable Risk Factors
As the name suggests, non-modifiable risk factors cannot be changed (ethnicity being a prime example of this), but they can be controlled.

Age – atherosclerosis occurs gradually over many years; as such, older adults would naturally have a greater predisposition to this condition.
Gender – males appear to have a greater risk of atherosclerosis than females; this is largely believed to be because of hormonal factors.
Family history – genetic factors are believed to be the strongest predictor for the development of cardiovascular diseases and other chronic illnesses. Those who have a first-degree relative who suffers from this condition are 50% more likely to develop heart disease-related conditions.
Ethnicity – those from a black, Asian and minority ethnic (BAME) have some of the highest rates of heart disease, which include strokes, hypertension, and atherosclerosis.
Management of Atherosclerosis
Atherosclerosis is rarely managed as a condition in its own right because the degree to which plaque is being deposited in the artery wall is extremely difficult to quantify outside of a clinical environment. Instead, other related factors are closely monitored to determine the severity of atherosclerosis; these include:
- Heart rates
- Blood pressure
- Cholesterol profiles
In the first instance, the management of atherosclerosis will require a lifestyle change in which high-fat foods will need to be replaced with a lower fat option. If the client or patient isn’t aware of how to go about cutting out high-fat foods from their diet then a fitness professional should provide guidance where appropriate and always within the scope of their qualifications.
Exercise and physical activity will also form an integral part of the new lifestyle and should be performed under close supervision by an appropriately qualified person.
Medication can also be prescribed to help manage this condition; generally, the group of medications referred to as ‘statins’ are the most widely prescribed for treating atherosclerosis. They have relatively few short-term or longer-term side-effects, and have consistently demonstrated strong results in reducing atherosclerosis.
Surgical interventions are occasionally used as a last resort with one of the most common being an angioplasty. This is a technique whereby the obstructed blood vessel is mechanically widened using a wire-like object and balloon (balloon catheter).
Exercise Recommendations
While the use of exercise as a means of treating or reversing atherosclerosis has been questioned, research does suggest that the benefits of exercise on other cardiovascular variables will help to manage the condition and prevent it from worsening. The patient’s total blood flow in the diseased limb is unlikely to change significantly following the uptake of exercise; however, patients are likely to experience cardiovascular and respiratory adaptations which promote the better utilisation of oxygen and increase their walking threshold to the point at which pain sets in.

Aerobic
Aerobic exercise also has a wide range of additional physiological adaptations, including:
- Reduced blood pressure
- Increased HDL concentration
- Increased fibrinolysis – removal of small blood clots
- Increased stroke volume
- Decreased resting and exercising heart rate, resulting in a longer diastole
- Increased end-diastole volume (volume of blood in the heart at the end of diastole
- Increased cardiac output
- Increased haemoglobin concentration within the red blood cells
- Increased tone in the smooth muscle of the artery wall
Since aerobic exercise improves the efficiency and resilience of the cardiovascular system, regular participation can help to reduce the risk of further cardiovascular complications and increase the survival rate if repeat episodes do occur.
During exercise, it is important to monitor the heart rate, as most patients will have a safe upper limit above which exercise may become hazardous. It is, therefore, vital that intensity is monitored using RPE or by heart rate monitors, and that exercise prescription should start at a low intensity and be largely focused on cardiovascular training approaches.
In patients who experience intermittent claudication, a validated pain scale ranging from 0 to 4 may be used to assist patients in determining progress (0= no pain, 1= onset of pain, 2= moderate pain, 3= intense pain, 4= maximal pain). The patient and exercise professional should monitor the time between the start of exercise and the onset of pain to determine progress surrounding the claudication.
Cardiovascular
Regular cardiovascular exercise has been found to increase vasodilation and reduce arterial pressure and damage. Most cardiovascular programmes for atherosclerotic patients should focus on walking with progression aimed at improving the pain response associated with walking speeds and increasing walking times.
By deferring the point at which pain sets in during walking activities, the patient is likely to become more functionally independent in their daily activities.
A secondary goal of cardiovascular exercise, although equally important, is that of reducing other risk factors, which may exacerbate the condition.
Flexibility
Flexibility and mobility exercise can maintain joint ROM, but need to be adapted to the individual condition.
Only passive stretches should be performed and their duration should be reduced to prevent the stretch reflex (isometric muscle contraction) from causing blood pressure to spike.
Resistance
Resistance training programmes should only begin if a low-level aerobic exercise programme has been followed comfortably, and more importantly asymptomatically, for more than 3 months.

Isometric exercises should be avoided due to their effects on blood pressure, especially with patients who also have hypertension.
Additionally, overhead exercises and those which place the head and shoulders in a position lower than the heart should be risk assessed as to their suitability for the patient. In most cases, it is much simpler and safer to simply exclude these from the programme.